Table of Content
- Introduction to High Altitude Sickness
- What is Altitude Sickness (AMS)?
- What Counts as High Altitude?
- Common Symptoms of Altitude Sickness
- Complications: HAPE and HACE
- Causes of Altitude Sickness
- How to Prevent Altitude Sickness
- What is Hypothermia?
Some Fact about High Altitude sickness
Generally, trekkers come for high-altitude Himalayan treks and they are not aware of altitude sickness. Trek the Himalayas has collected some information and our experience to share about altitude sickness to help Himalayan trekkers. Altitude sickness generally refers to a condition known as Acute Mountain Sickness (AMS). It affects people in areas of high altitude, which means areas at around 2,500m above sea level. Altitude sickness is more common, and becomes more severe, with increasing altitude.
About Altitude Sickness:-
If you ascend to an area of high altitude, you are likely to experience some form of altitude sickness. Usually, the symptoms are mild and will improve if you descend. Altitude sickness is most likely to affect you if you ascend quickly, especially at a rate of more than 500m per day or if you don’t allow yourself time to get used to the height (acclimatise).
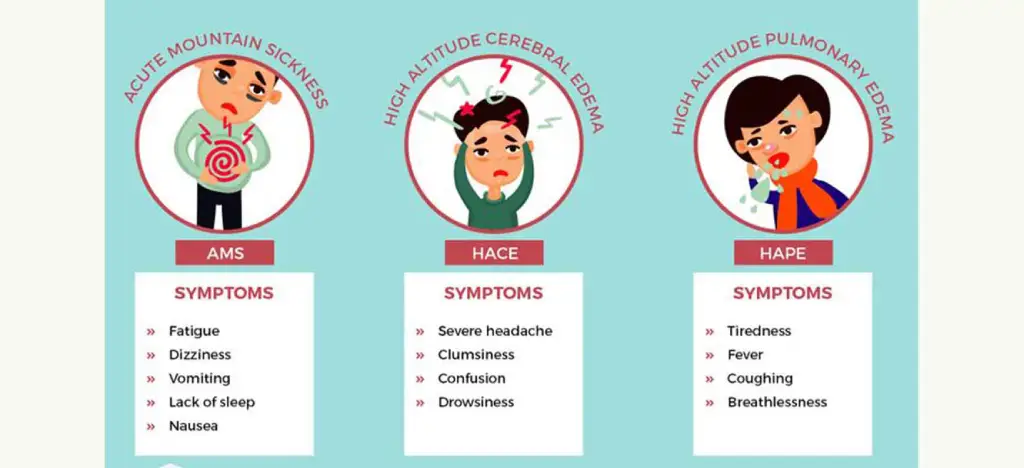
Acute mountain sickness (AMS) is the most common and mildest form of altitude sickness. If you go on a climbing expedition or stay in an area of high altitude, you may develop AMS. High-altitude pulmonary oedema (HAPE) and high-altitude cerebral oedema (HACE) are much more severe forms of altitude sickness. They usually affect you only if you are at a very high or extreme altitude.
What Counts As High Altitude?
- High altitude treks refers to heights that are between 1,500 and 3,500m above sea level.
- Very high altitude is from 3,500 to 5,500m above sea level.
- Extreme altitude is from 5,500 to 7,500m above sea level.
Symptoms of Altitude Sickness
You may notice symptoms of altitude sickness about six to 24 hours after you’ve arrived at an area of high altitude. However, this varies from person to person and will depend on the speed of your ascent. If you’ve been climbing or ascending slowly, the onset of your symptoms will be more gradual.
If you have altitude sickness in its mildest form (AMS), you may:
- Have a headache
- feel tired
- feel sick or vomit
- lose your appetite
- feel dizzy
- have difficulty sleeping
Symptoms of AMS usually start to ease within about two days as your body acclimatise to the high altitude, particularly if you don’t ascend any further. If your symptoms get worse, the best thing you can do is descend as quickly as possible. Some medications can help ease your symptoms and treat complications, but only descending will deal with the cause.
Complications of Altitude Sickness
If you ascend to an area of high altitude too quickly and don’t allow your body time to acclimatise, you may develop a serious form of altitude illnesses such as HAPE or HACE. These conditions are rare, but potentially fatal if you don’t descend immediately and receive treatment.
HAPE occurs when fluid builds up in your lungs. Symptoms usually develop between two and four days after a rapid ascent over 2,500m. You may:
- Have a dry cough
- Feel breathless at rest
- Have a fever
- Feel confused
- Have pink or bloody spit
- Have a bluish tinge to your skin, lips and nails (cyanosis)
If you have severe symptoms of HAPE, you may gasp for breath and make gurgling sounds when you breathe. HAPE can occur by itself or in conjunction with HACE. HACE occurs when excessive fluid collects in your brain, causing it to swell. Fewer than two per cent of people with altitude sickness develop HACE and it rarely occurs below 4,000m. If you have HACE you may:
- Have a severe headache
- Feel very confused
- Lose coordination
- Have blurred or double vision
- Notice changes in your behaviour – for example, you may feel irritable or be unhelpful
- Lose consciousness
- Hallucinate (see, hear, feel and smell odd things that aren’t there)
- Fall into a coma (this is rare)
The symptoms of HACE may progress rapidly from mild to life-threatening within a few hours. If you have these symptoms, you should descend to a lower altitude as soon as possible and seek urgent medical advice.
You may develop other symptoms at high altitudes. For example, your face, arms or legs may swell up (peripheral oedema). This usually lasts a few days and then disappears. At altitudes of 5,000m and over, tiny blood blisters can form at the back of your eye (retinal haemorrhages), but you may not notice any symptoms and they only occasionally interfere with your vision.
Causes of Altitude Sickness
At high altitudes, the air is at a lower pressure than it is nearer sea level. This makes it harder to get oxygen out of the air you breathe in, and into your bloodstream. Your body responds by increasing your breathing and heart rate.
Certain factors may make you more likely to develop altitude sickness; for example, if you:
- Have had altitude sickness before
- Do strenuous activity or exercise at high altitude
- Rapidly ascend to high altitude
- Have a lung infection
If you have diabetes, or a heart or lung condition, you should check with your GP before travelling to places at altitude. Many people with such conditions can cope very well but certain severe conditions may mean it’s unwise for you to travel to, or climb in, areas of high altitude.
Prevention of Altitude Sickness
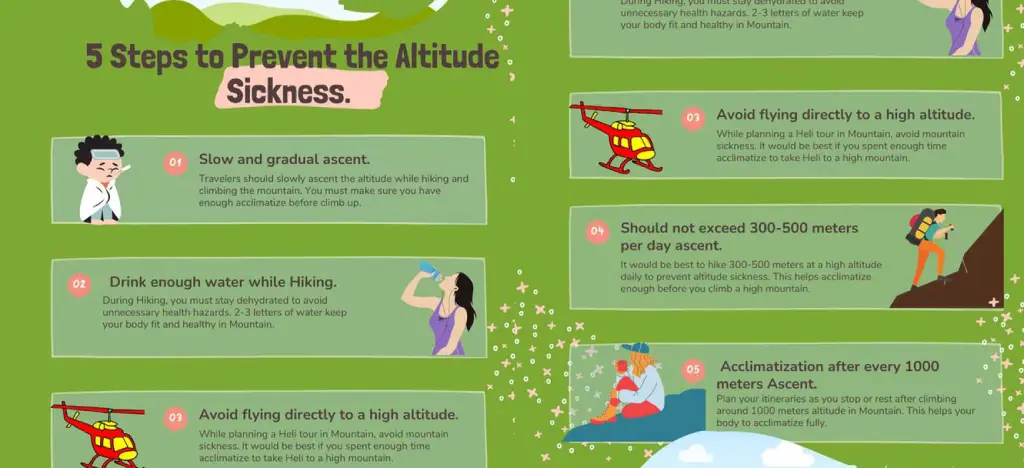
There are several steps you can take to prevent altitude sickness. Wherever possible:
- Acclimatise yourself to high altitudes by slowly ascending over several days – if possible, don’t sleep at an altitude more than 300m higher than the previous night
- Make sure you drink enough fluids
- Eat high-carbohydrate foods
- Don’t do any strenuous exercise or activity for the first few days after you arrive at a high altitude and have rest days planned if you are ascending further
There are several medications you can use to prevent the symptoms of altitude sickness. A medicine called acetazolamide is being used more and more, but it isn’t, however, a substitute for acclimatisation. Alternatively, you may be able to take a medicine called dexamethasone. This is effective for both the prevention and treatment of altitude sickness and can prevent HAPE if you have suffered from severe altitude sickness before. If you have had HAPE before, your doctor may prescribe you a preventive drug such as nifedipine.
Note:- Ask a doctor from a travel clinic about these medicines because you can only get them on prescription. Always ask your doctor for advice and read the patient information that comes with your medicine.
What is Hypothermia?

The second most common sickness in the mountains is Hypothermia. The body maintains a relatively stable temperature whereby heat production is balanced by heat loss. Normally, the core body temperature (when measured rectally) is 98.6 degrees F or 37 degrees C. When the outside environment gets too cold or the body’s heat production decreases, hypothermia occurs (hypo=less + thermia=temperature). Hypothermia is defined as having a core body temperature of fewer than 95 degrees F or 35 degrees C.
Body temperature is controlled in the part of the brain called the hypothalamus, which is responsible for recognizing alterations in the body temperature and responding appropriately. The body produces heat through the metabolic processes in cells that support vital body functions. Most heat is lost at the skin’s surface by convection, conduction, radiation, and evaporation. If the environment gets colder, the body may need to generate more heat by shivering (increasing muscle activity that promotes heat formation). But if heat loss is greater than the body’s ability to make more, then the body’s core temperature will fall.
As the temperature falls, the body shunts blood away from the skin and exposure to the elements. Blood flow is increased to the vital organs of the body including the heart, lungs, kidney, and brain. The heart and brain are most sensitive to cold, and the electrical activity in these organs slows in response to cold. If the body temperature continues to decrease, organs begin to fail, and eventually, death will occur.
During good weather conditions, you tend to ignore the weather. If it’s sunny, you’ll probably feel warm and neglect to carry the proper clothing necessary in the event of inclement weather. You may even lack food and rudimentary shelter and equipment necessary for survival in an emergency.
If the weather changes suddenly, or you or a member of your party is injured, you may find yourself unprepared to face adverse conditions. Hypothermia symptoms usually begin slowly. As you develop hypothermia, your ability to think and move often becomes clouded. You may even be unaware that you need help. As your thought process is impaired, you fail to realise that you are becoming colder. Once you get cold, it can be very difficult to get warm again. Someone with hypothermia is likely to have frostbite as well.
The key hypothermia symptom is an internal body temperature below 95º F (normal is 98.6º F).
Usually, everyone thinks about hypothermia occurring in extremely cold temperatures, but that doesn’t have to be the case. It can happen anytime that you are exposed to cool, damp conditions. Older people are more susceptible to hypothermia.
Two things to remember about hypothermia are that
- You don’t need to be experiencing sub-zero temperatures to encounter hypothermia and
- Your judgement will be impaired making you much more likely to experience an accident.
If you, or someone in your group, become hypothermic, take immediate action before it becomes a severe emergency!
Hypothermia symptoms include:
- Uncontrollable shivering (although, at extremely low body temperatures, shivering may stop)
- Weakness and loss of coordination
- Confusion
- Pale and cold skin
- Drowsiness: especially in more severe stages
- Slowed breathing or heart rate
If not treated promptly, lethargy, cardiac arrest, shock, and coma can set in. Hypothermia can even be fatal.
Hypothermia signs that can be observed by others:
- Slowing of pace, drowsiness, fatigue
- Stumbling
- Thickness of Speech
- Amnesia
- Irrationality, poor judgement
- Hallucinations
- Loss of perceptual contact with the environment
- Blueness of skin
- Dilation of pupils
- Decreased heart and respiration
- Stupor
- Death
Victims need IMMEDIATE help if the following symptoms are present. If you observe ANY of these hypothermia symptoms or signs in yourself or anyone in your party, seek immediate help:
- Poor articulation of words
- Disorientation
- Decrease in shivering followed by the rigidity of muscles
- Cyanosis (Blueness of Skin)
- Slowness of pulse, irregular or weak pulse





.webp)









.webp)
.webp)


.webp)
.webp)

.webp)


